23 آگوست Living with Ulcertative Colitis
OVERVIEW
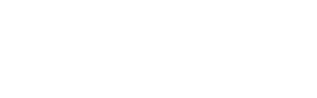
Ulcerative colitis is a type of inflammatory bowel disease (IBD) that affects the large intestine, also known as the colon.
In patients with ulcerative colitis, the lining of the colon becomes inflamed and develops ulcers (tiny open sores). This combination of inflammation and ulcers leads to long-lasting discomfort that can be debilitating and may even lead to life-threatening complications. Because ulcerative colitis is a chronic disease, symptoms may not develop immediately.
Unlike Crohn’s disease, another type of IBD that can affect any part of the gastrointestinal track, ulcerative colitis affects only the colon.
Scientists have yet to find a cure for ulcerative colitis; however, there are treatments that can reduce symptoms. For some patients, these treatments can lead to long-term remission (periods with little or no symptoms).
SYMPTOMS
The signs and symptoms of ulcerative colitis can vary from patient to patient, depending on the severity of the condition. About half of ulcerative colitis patients have mild symptoms.
The most common symptoms of ulcerative colitis include abdominal pain and blood or pus in diarrhea. Other symptoms include the following:
- Anemia — a lack of enough healthy red blood cells, which provide oxygen
- to body tissues
- Low energy and fatigue
- Weight loss
- Loss of appetite
- Bleeding from the rectum
- Sores on the skin
- Joint pain
- Delayed growth and development in children
The symptoms of ulcerative colitis tend to come and go. That is, patients often have periods in which symptoms flare up followed by periods in which they may have no symptoms at all. While these periods of remission can last for months or even years, symptoms usually return at some point.
DIAGNOSIS
Because ulcerative colitis shares symptoms with a number of other conditions, a doctor is likely to diagnose ulcerative colitis only after ruling out other possible causes of those symptoms.
Doctors may use a combination of the following tests to make a proper diagnosis:
Blood tests: A doctor may order blood tests to check for anemia, infection or the presence of certain antibodies. While these tests help in the diagnosis of ulcerative colitis, they cannot tell with certainty if a patient has the condition.
Stool samples: Doctors use these tests to look for white blood cells in patients’ stools — a sign of inflammatory diseases like ulcerative colitis. Stool samples also help doctors rule out other conditions with similar symptoms as ulcerative colitis. For example, certain bacterial infections can cause diarrhea.
Colonosopy: In a colonoscopy, a doctor uses a thin, flexible tube with a light and camera attached to get a view of the entire colon. During this exam, the doctor also may take a small sample of tissue, or biopsy, for lab testing.
Sigmoidoscopy: This exam may take the place of a colonoscopy if the colon is too severely inflamed. Sigmoidoscopy involves a thin, flexible tube that gives the doctor a view of the sigmoid, the part of the colon closest to the rectum. However, it may miss problems farther up the colon.
Imaging tests: An X-ray of the abdominal area may be used to rule out certain conditions, such as toxic megacolon, that may be causing severe symptoms. CT scans of the abdomen or pelvis are used to spot complications of ulcerative colitis or Crohn’s disease. CT scans also can reveal the level of inflammation in the colon.
TREATMENTS
As there is no cure for ulcerative colitis, the main goal of treatment is to reduce the inflammation that causes symptoms.
Treatment of ulcerative colitis typically involves a combination of approaches, including medication and lifestyle changes. In some cases, patients may require surgery.
Medications
Doctors use a number of different medications to control inflammation and symptoms of ulcerative colitis. The medications that work for one patient may not work for another, so if you have ulcerative colitis, your doctor may prescribe multiple medications before finding the one that works best for you.
The following categories of medication are used to treat ulcerative colitis:
Anti-inflammatory medications: These medications are often part of the first line of treatment. They are used to reduce inflammation and to maintain remission. Anti-inflammatory medications used to treat ulcerative colitis include sulfasalazine (brand

name Azulfidine), mesalamine (Asacol, Lialda and others), balsalazide (Colazal) and olsalazine (Dipentum). Corticosteroids are also used to control inflammation in patients with ulcerative colitis. Some of these medications carry risks for serious side effects, so speak with your doctor before starting any new treatment.
Immune system suppressors: Like anti-inflammatory medications, immune system suppressors also reduce inflammation. However, instead of treating the inflammation itself, immune suppressors target the immune system. As the name implies, these medications suppress the immune system response so it does not cause inflammation to continue. Immune system suppressors used to treat ulcerative colitis include azathiprine (brand names Azasan, Imuran), mercaptopurine (Purinethol), cyclosporine (Gengraf, Neoral, Sandimmune), infliximab (Remicade) and adalimumab (Humira).
Other medications: While the main goal of ulcerative colitis treatment is to reduce inflammation at the root of the disease, patients also need symptom relief. Depending on the type and severity of ulcerative colitis symptoms, a doctor may prescribe antibiotics, anti-diarrheals, pain relievers or even iron supplements.
It may take some trial and error to find which foods aggravate symptoms and which foods ease symptoms. Many people with ulcerative colitis find that the following suggestions have helped them:
Limit dairy: Some ulcerative colitis patients find that dairy products aggravate symptoms. If you have ulcerative colitis, try cutting dairy out of your diet to see if symptoms improve.
Try changing fiber consumption: For most people, a healthy diet usually includes high-fiber foods like fruits, vegetables and whole grains. However, for those with ulcerative colitis, fiber can worsen symptoms like diarrhea, pain and gas. Discuss your fiber intake with your doctor if fruits and vegtables bother you.
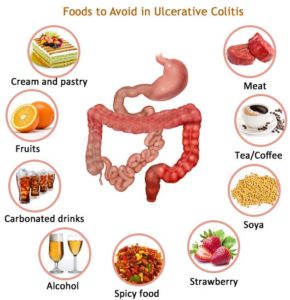
Eliminate problem foods: Avoid eating foods that seem to aggravate symptoms. For some, such foods may include those that cause gas, such as beans, cabbage and brocolli or caffeine and carbonated drinks.
Eat small meals: Instead of eating two or three large meals in a day, try eating five or six smaller meals.
Drink plenty of liquids: Make sure your getting enough liquids each day, particularly water. Other beverages, such as those with caffeine or carbonation, may make symptoms worse.
Ask your doctor about multivitamins: Patients with ulcerative colitis don’t always get the nutrients they need. The condition itself can limit one’s ability to absorb nutrients, and the limited diet many patients require may mean those patients aren’t getting much needed nutrients in the first place. If you have ulcerative colitis, talk to your doctor about whether you may benefit from taking vitamin and mineral supplements.
Talk to a dietitian: Because a great deal of ulcerative colitis management requires diet changes, it may help to work with a registered dietitian.
Surgery
If lifestyle changes and medications fail to ease symptoms of ulcerative colitis, doctors may recommend one of two surgery options, depending on various factors, such as the extent of disease and patient age and overall health. Both options involve removing the colon.
In the first surgery, which was more common in the past, the entire colon and rectum are removed. The patient then wears a small bag over an opening in the abdomen (ileal stoma) to collect stool.
Now, with new surgical techniques, patients have another option. Like the first, this procedure involves removing the entire colon, but instead of the small bag attached to the abdomen, this second procedure puts a pouch inside the small bowel attached to the anus. This allows the patient to expel waste in a more normal fashion.
CAUSES
It’s not entirely clear what causes ulcerative colitis, but researchers have an idea of what does not cause it. Stress was once thought to be the main cause, but now it seems that stress merely makes symptoms worse.
Today, when it comes to studying the causes of ulcerative colitis, researchers are focused on the immune system and genetics.
Some researchers think that viral or bacterial infections may trigger ulcerative colitis. More specifically, they suspect that the large intestine become inflamed because the immune system is trying to fight off the invading virus or bacteria. Other scientists think the immune system is involved in ulcerative colitis in another way — that inflammation is triggered by an autoimmune response in which the immune system mistakenly attacks tissue when there is no outside invader.
Even though most ulcerative colitis patients do not have a family history of the condition, people have an increased risk for ulcerative colitis if they have a parent or sibling with the disease. Therefore, some scientists think that genes may play a role in the development of ulcerative colitis.
GETTING HELP
For some, it can be hard to tell if their bowel symptoms are something simple that will pass or if they need the attention of a doctor. It may be time to visit your doctor if you notice a continued change in your bowel routine or if you have any ulcerative colitis symptoms, such as the following:
- Abdominal pain
- Bloody stools
- Continuing periods of diarrhea that don’t get better with over-the-
- counter medications
Unexplained fever that lasts more than a couple days
While ulcerative colitis typically isn’t a deadly disease, complications associated with ulcerative colitis can be life-threatening.
Your family doctor will likely be the first person you see after noticing symptoms of ulcerative colitis. But that doctor might eventually send you to a specialist called a gastroenterologist.
Before seeing a gastroenterologist, it’s a good idea to prepare, particularly because you may not have a lot of one-on-one time with this specialist. It might be a good idea to write down a list of things you want to tell the gastroenterologist or that the gastroenterologist might need to know. This list may include:
- Your symptoms
- Personal information
- Medical information
- All medications, vitamins and supplements you are taking
- Any questions you have
RELATED INFORMATION
Ulcerative colitis is one of many conditions known as inflammatory bowel diseases (IBD), which are characterized by a chronic immune response and inflammation of the gastrointestinal tract. Crohn’s disease is another common form of IBD.
According to the CDC, IBD is the condition behind more than 700,000 physician visits and 100,000 hospitalizations. IBD also accounts for disability in an estimated 119,000 patients.
As much as 25 percent of patients with ulcerative colitis will require surgery over the long term.
LIVING WITH

Living with a chronic condition like ulcerative colitis not only takes a physical toll, but also can affect your emotional health. The pain, discomfort and persistent need to use the toilet can make center a patient’s life around this disease. Even mild symptoms like gas can keep people from making public appearences. For some patients, ulcerative colitis keeps them from even leaving the house. Feelings of isolation, embarrassment and anxiety can build up and may even lead to more serious mental health issues like depression.
For these reasons, many ulcerative colitis patients need support. For some, support simply comes from family. Other patients may turn to support groups. Some patients find it helpful to see a mental health professional who has experience dealing with patients with inflammatory bowel disease.
Ask your doctor for suggestions if you need help coping with the emotional aspect of living with ulcerative colitis.